NORFOLK, Va. (WAVY) – “Transformative” and “breakthrough” are two words tossed around frequently when it comes to health care. A procedure available at Sentara Norfolk General and Riverside hospitals appears to check both boxes.
MRI-guided focused ultrasound is getting profound results for patients with tremor from Parkinson’s disease, and in some cases, the results are immediate.
According to the Parkinson’s Foundation, 70-90% of people with PD experience a tremor at some point, and it is often the first motor symptom.
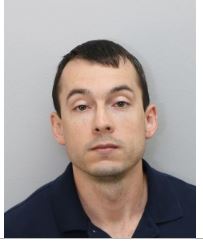
Michael Newby, 58, of Chesapeake came to Sentara Norfolk General last week with Parkinson’s tremor in both hands. He also came with high expectations.
“I want to make things a little bit easier in life,” he said in a pre-op interview, “especially simple things like shaving, taking a bath, getting dressed.”
The procedure treats just one side at a time, and this one will target only his left hand. First, neurosurgeon Shannon Clark put Newby through some exercises to get a baseline.
Newby’s trembling left hand struggled to touch her nose and the tip of her finger. Some writing tests measured how smoothly he can draw.
Newby then entered a room adjacent to an MRI machine with about eight people. Half are healthcare providers, half are technicians from Insightech, the company that makes the machine.
Clark fit Newby’s head with a special bracket to ensure it remained steady for the 45 minutes he would be inside the machine.
The team made some last minute preparations and then slid Newby into the MRI.
Clark explained to WAVY how she does brain surgery without the need for incision.
“It’s ablating, creating a burn in the brain, kind of like a really controlled small burn to disrupt the circuit that’s making them have tremor,” she said.
The temperature reaches about 150 degrees F at its peak.
“In general, patients have 70% to 80% improvement in their tremors, that are fairly long-lasting,” Clark said. “Occasionally, some patients will have tremor recur, but not to the extent of the previous degree.”
“I’m feeling good,” Newby said as he emerged from the MRI. He said lying still was the hardest part – just like any MRI.
“I felt the heat and the cold” during the procedure Newby said. “I could feel it when I was in the machine, I could feel the difference. This side was shaking a little bit, but this side was completely calm, so it was unreal.”
He performed the same tests post-op to gauge the improvement.
Newby touched Clark’s finger much more easily.
“Very steady,” Clark said. “Compared with the pre-op, he’s also faster and can get to the target with the first try. I think it’s a significant improvement.”
His writing test drawing a spiral and straight lines were more fluid now, with fewer stops and starts.
For comparison, Newby raised his trembling untreated right hand up to his steady left hand. He said getting the same procedure for the right hand is already on his to-do list.
“I’m very pleased.”
It’s important to note that the ultrasound procedure works only on upper body tremor, but it works for both Parkinson’s and essential tremor. It does not treat Parkinson’s dementia. Provided there are no complications, it requires just one follow-up visit two weeks after the operation.